1) Big Benefits, Overlapping Roles
Vitamin D: A hormone-like “vitamin” with wide reach
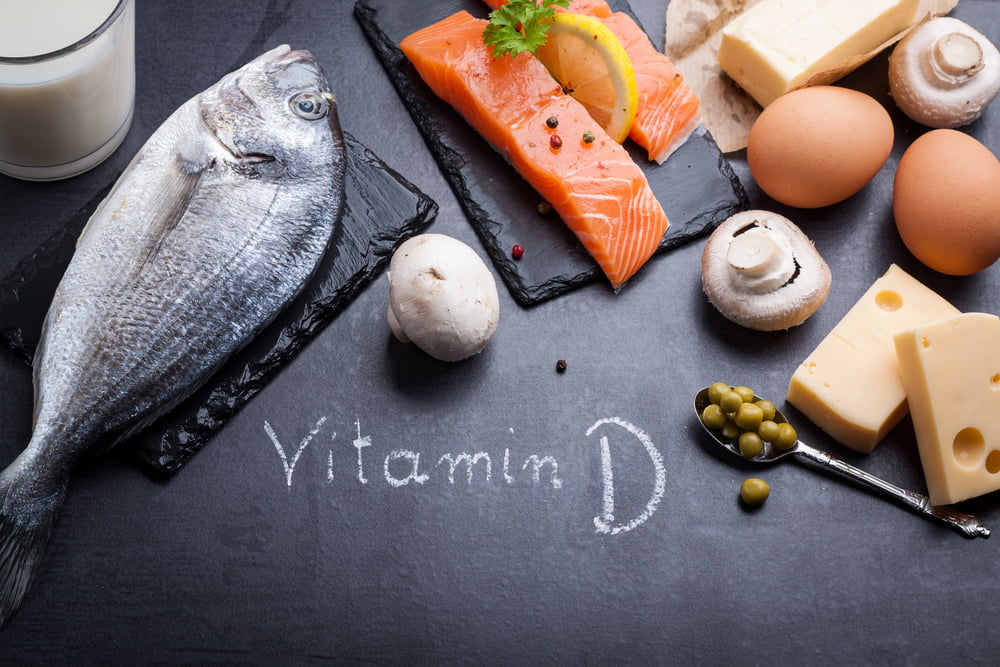
Long known for building strong bones, vitamin D also influences cardiovascular health, immune resilience, and metabolic wellness. Technically a steroid hormone, it helps your body absorb and regulate calcium and phosphorus. While your skin can make vitamin D from sunlight, real-world factors—season, latitude, skin tone, sunscreen, time indoors—often limit natural production. Food sources (e.g., fatty fish, eggs, dairy, beef) help, but diet alone is tough for many people. That’s why supplements are common—when people remember to take them.
Omega-3s (EPA & DHA): Built into every cell you own
EPA and DHA—marine omega-3 fats from fish, krill, and algae—live in cell membranes throughout the body. They support flexible, well-functioning cells and healthy signaling in your heart, blood vessels, immune system, eyes, and brain. These fats are among the most researched nutrients on earth, with tens of thousands of papers exploring their effects.
2) Sky-High Interest, Widespread Shortfalls
Consumers care—but intake still lags
Surveys show omega-3s are a top “must-have” nutrient, yet many people can’t name their key benefits—and even fewer get enough from food. Vitamin D ranks among the most popular supplements (second only to multivitamins in some polls), but deficiency remains common enough that U.S. dietary guidelines label it a “nutrient of public health concern.”
How much vitamin D is “enough”?
Guidance varies. The Institute of Medicine set 600 IU/day for most children and adults and upped the safe upper limit to 4,000 IU/day, noting no evidence of harm at that level. Many experts argue a higher intake is often needed for optimal bone and whole-body health—especially with limited sun exposure.
Omega-3 status is low across the globe
Population studies using the Omega-3 Index (EPA+DHA in red blood cells) reveal many regions—particularly the Americas, parts of the Middle East, and India—have low status consistent with modern dietary patterns. Sub-optimal omega-3 levels are linked with higher cardiovascular risk, underscoring the need to close the intake gap.
3) Vitamin D + Omega-3s: A Potential Power Pair
Inside the VITAL trial
Can taking both nutrients move the needle on major diseases? The landmark VITAL study set out to find out by testing 2,000 IU/day of vitamin D₃ and 1,000 mg/day of marine omega-3s (EPA+DHA)—alone and together—versus placebo in more than 25,000 U.S. adults. Primary outcomes include cancer, heart disease, stroke, and even late-life mood. As results continue to emerge, VITAL is poised to clarify where these nutrients shine—individually and in combination.
4) Know Your Numbers: Simple At-Home Testing
Omega-3 Index: See your EPA & DHA status
A quick finger-prick test measures EPA and DHA as a percentage of total fatty acids in red blood cells—the Omega-3 Index. It reflects long-term intake (not just last night’s salmon) and helps you personalize diet and supplement decisions.
Vitamin D: Test, adjust, repeat
Vitamin D can be checked just as easily with a small blood spot sample—no lab draw or doctor’s visit required. Because sun, season, and genetics vary, testing lets you tailor your intake and track progress over time.
Bottom line
Vitamin D and omega-3s are foundational for whole-body health—and many of us fall short. Consider a food-first approach (fatty fish, fortified foods, sensible sun) supported by smart supplementation when needed. Most importantly, test your levels, fine-tune your plan, and re-test to make sure your habits are actually delivering results.